Extreme variance in healthcare costs is no surprise. In fact, it is one of the most discussed problems pertaining to the healthcare industry. Yet, there have been no major strides to tackle this problem in recent years. To address and mitigate these cost fluctuations, the data science team at Medxoom has developed a set of models that can aid in predicting and optimizing costs for a variety of health plans and self insured employers.
Through a series of articles, we will discuss the need for predictive modeling, the creation of our healthcare pricing models, and how health plans can use these models and other features of the Medxoom platform to reduce their total healthcare spending.
Using predictive models to lower healthcare costs
A 2019 study showed that 66.5% of all bankruptcies were tied to medical issues.
Not only does the cost of healthcare keep rising, but transparency around those prices is largely inaccessible to consumers. This combination hinders consumers from choosing affordable care and increases a health plan’s overall costs. The need for price transparency has never been more urgent than it is today.
To create a solution for consumers and health plans alike, the Medxoom data science team has created a set of predictive models that can be tailored to aid in estimating future healthcare costs specific to various scenarios. Some of these models are built upon the Centers for Medicare and Medicaid Services (CMS) structure for provider and hospital reimbursements. CMS is the largest payer for healthcare in the United States. Thus, many payers in the industry look to CMS rates as benchmarks to set their own reimbursement rates.
Frequently the relationship between CMS and private payer payments are simple linear models, while in other instances advanced machine learning models may be required to determine the relationship. Utilizing these models to more accurately steer consumers to providers with more predictable, lower pricing almost always allows health plans to reduce their total healthcare spending.
Some of the Medxoom models are characterized through the examples below.
The Provider Experience
Health plans generally try to get the best possible reimbursement rates for their members. They do this through pre-negotiating rates for a specific provider’s services. Once the rates are determined, the health plan tries to steer their members to these “in-network providers.” Members are then able to get a better rate for their healthcare as opposed to going to an “out-of-network” provider.
However, when a member needs to see a provider, typically their healthcare services are billed using a fee for service model. This is a simple method using each service as a line item with a corresponding price. Members traditionally have little insight into the exact costs associated with a specific service. CMS may set the benchmark but there can still be an extreme amount of variance (see Figure 1). Thus, it is difficult for members to shop around and get an accurate understanding of what both their health plan and themselves may have to pay for each visit.
This is where the Medxoom models can help. Demonstrating the relationship between Medicare and private payer costs allows members to see variance in price for their healthcare options and choose providers that offer the best price.
For example, Sam is a member of an employer sponsored health plan that is currently using Medxoom’s Predictive Pricing technology. Sam needs to schedule an eye exam with a provider in the area. Within the health plan’s app Sam is able to search various providers and see cost and quality estimates for the desired service. This experience allows Sam to reduce overall healthcare costs by viewing the price variance for this particular service and then choosing the best priced provider.
The Hospital Experience
Predictive pricing within the hospital setting can be more complicated. When members receive care in this environment it can be inpatient care, outpatient care, or emergency services. Furthermore, members are likely receiving many services in one visit. This means that healthcare costs when billed using the fee for service method can become exorbitant.
Medicare has worked to streamline this pricing problem through diagnosis-related groups (DRGs). These are bundled payments for hospital services, sorted by diagnosis and severity. In some instances, bundled payments in both the public and private sectors have expanded to include physicians, post-acute care (PAC) providers, and hospitals.
Our predictive pricing technology is able characterize a private payer’s price relative to Medicare. For example, our previous member Sam needs to get a knee replacement. Using Medxoom’s predictive pricing technology Sam is now able to shop for bundled procedures. When reviewing the cost of a knee replacement, Sam can see the out-of-pocket costs associated with the procedure – from the actual surgery to the rehabilitation that comes afterward. This access to data and guidance from the health plan ensures that Sam picks the most affordable and high quality options.
So how does all of this help members and health plans? Having a better understanding of hospital and provider level prices for the commonly ‘shopped for’ procedures feeds our pricing engine and allows us to suggest strategies that health plans can adopt to achieve significant savings, both immediately and several years down the line. Furthermore, the ability to shop for the most affordable and high quality options in healthcare services yields a better more consumer friendly healthcare experience for members.
Variation in Prices of Common Procedures
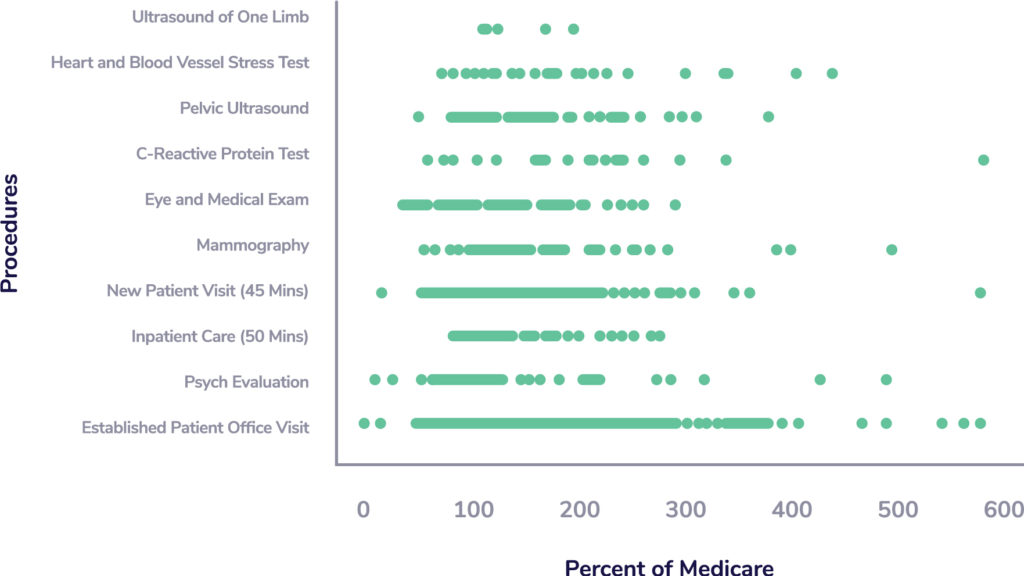
Figure 1: Variation observed in prices of common procedures as a percentage of Medicare in a Northeast focused Private Insurer.
To download this blog post in a PDF, please click here.